Last updated on October 5th, 2024 at 04:46 pm
After the leg fracture and plaster cast removal, the patient’s most important concern is when they will resume walking. For this, they have to follow proper tibia fibula fracture rehabilitation protocol. This article will teach us about step-by-step physiotherapy exercises after a tibial shaft fracture. However, we suggest you perform these exercises/protocols under the supervision of a qualified physiotherapist.
We have covered the rehabilitation protocol for each day, from day one, when the fractured leg is operated on, to the final day, when a person starts walking. So, let’s get started.
Table of Contents
Tibia fibula fracture physiotherapy rehabilitation
The tibial shaft fracture is among the most common long bone fractures. The management and prognosis of tibial shaft fractures are influenced by their location in the bone (proximal, middle, or distal third) and orientation (transverse, oblique, spiral, or comminuted).
So, it is essential to know the classification of tibial shaft fracture before we read further.
Classification of tibial shaft fracture
OA/OTA (Orthopaedic Trauma Association) is the commonly used classification system. It uses the alphanumeric system of classification based on the bone involved and the particular region of the bone involved.
The AO/OTA classification designates the region of the bone by a letter (A, B, C) for the severity of the fracture and a number (1, 2, 3) indicating increasing complexity and comminution1.
- The letter A is used to designate simple fractures,
- Letter B is for multi-fragmentary (comminuted) fracture and
- The letter C is designated for multi-fragmentary complex fracture, respectively.
- Type 1 represents mild to moderately severe fractures with superficial abrasions or contusions.
- High-energy fractures and deep abrasions with associated swelling comprise Type 2 injuries, often with impending compartment syndrome. Finally,
- Type 3 injuries include extensive skin and muscle damage, often caused by a crush injury, a severe fracture pattern, and compartment syndrome.
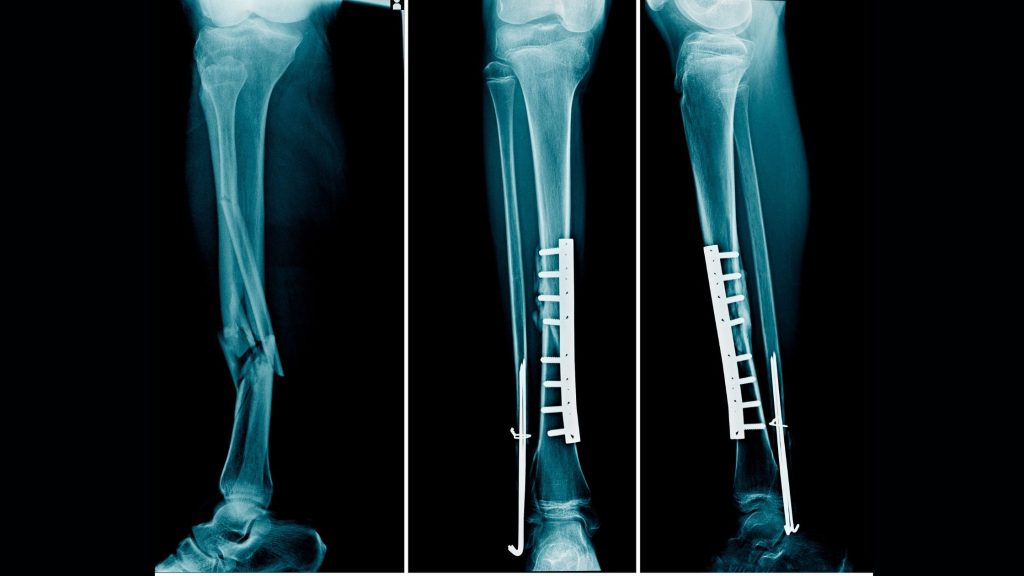
Surgical treatment for Tibia shaft fracture
Different types of fractures need different treatment approaches. A long leg cast can manage a closed, minimal displacement fracture (Type 1). Types 2 and 3 injuries almost always are managed operatively, with poorer outcomes related to the severity of soft tissue injury and fracture comminution1.
The surgical process involves open reduction internal fixation (ORIF) with an inter-medullary rod, intramedullary, or external fixation. After the surgery, the operated limb is immobilised for a month and a half. Immobilisation means making the operated limb not move. The purpose is to allow the surgical process to take its own time to heal without any disturbance.
The immobilisation process differs from doctor to doctor, but applying a plaster cast is the most common method. Most of the secondary complications develop during this long-term immobilization period due to a lack of proper care.
Complications of broken tibia and fibula
Most of the complications happen secondary to long-term post-operative immobilization.
- Disuse atrophy- Decrease in muscle bulk due to long-term rest.
- Muscle weakness
- Muscle contracture- Long-term immobility causes muscle contracture
- Joint stiffness- Muscle contracture,
in turn , leads to joint stiffness - Odema.
We can prevent such secondary complications by starting calculated movement and physiotherapy at the right time. Physiotherapy intervention prevents such complications by maintaining muscular and joint flexibility and blood circulation.
Tibia fracture physiotherapy rehab protocol
The goal of the surgical and rehabilitative team focuses on the return of a patient to their previous level of function, often in the setting of competing for short-term goals2. Before reaching the walking point, we must ensure all the walking components are intact. And this is the main motive of the protocol.
These include the flexibility of lower limb joints, like the hip, knee, and ankle joints. We also need to ensure sufficient strength of anti-gravity muscles and, most importantly, the weight-bearing capability of the affected limb. We need to start postoperative physiotherapy the very next day of the surgery after the leg is immobilised and the patient is still in bed.
Download: Tibia fibula fracture rehabilitation protocol pdf
In this article, we are going to learn just an overview of the protocol. However, if you need a complete step-by-step guide with clear illustration and instructions, then you can download the “Patients’ guide for tibia fibula fracture rehabilitation protocol“.
We will use this amount for the maintenance of the website so that I can keep giving you useful information.
Phase-I: Maximum protection phase
This
We have to be careful while selecting exercises during this period, the exercises should be static in nature with minimal or no movement at the surgical spot.

The exercises I would recommend is static quadriceps exercise (knee press) and ankle plantar flexion and dorsiflexion
Phase II: Range of motion and early strengthening
By this period, surgical pain should have subsided. Here, we have to begin exercises to improve joint range of motion and focus on strengthening all the muscles of the lower limb.
Importance of ROM exercises
Joint stiffness associated with surgical repair of periarticular fractures may have long-term effects on mobility, gait, and function. Knee stiffness, which is a reduced range of motion (ROM) resulting in functional limitations, can impact normal leg swing and ability to ascend and descend stairs as well as rise from a seated position, particularly when entering or exiting a vehicle2.
The limited extension may result in a limp, quadriceps strain, functional leg-length shortening, and patellofemoral pain, thus compounding the resulting dysfunction2.
A few of the recommended ROM exercises are knee bending exercises and hip abduction, as shown in the figure.


Importance of strengthening exercises
Muscle weakness around the thigh, knee and lower leg are very common after a tibial fracture. Weakness is actually secondary to the long term rest and immobilization period.
Home-based strength-training regimens moderately but significantly improve strength, balance, and functional mobility. Additionally, strength training provides a long-term reduction in patients’ perceived difficulty completing activities of daily living (ADLs) compared to controls2. Strength training starting even as late as 6 months post-fixation can provide significant improvement of functional outcomes for an extended period of time even beyond the end of treatment.
Phase-III: Progressive strengthening
Early weight-bearing protocols2:
| Injury type | Common fixation methods | Recommendation for initial weight bearing |
| Tibial shaft fracture | External fixation | Immediate weight bearing as tolerated |
| Intramedullary fixation | Immediate weight bearing as tolerated | |
| Comminuted/high-grade tibial fracture | ORIF | NWB for 6–12 weeks |
| External fixation | Conflicted, likely support some duration of NWB | |
| Intermedullary fixation | Immediate weight bearing as tolerated |
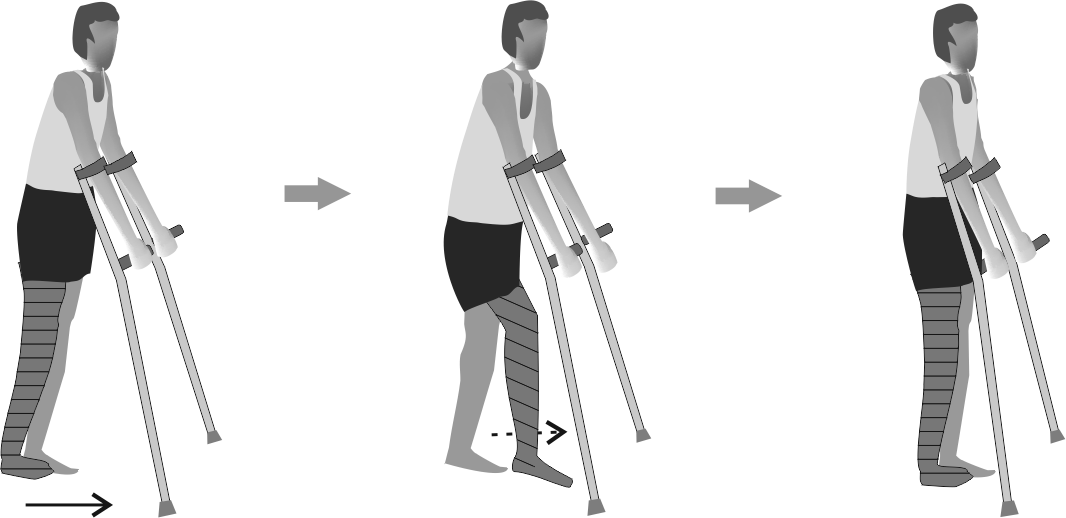
Start partial weight-bearing exercise using crutches. Observe the gait pattern and teach the correct gait pattern.
Phase-IV: Advanced strengthening
During this phase, we need to start full weight-bearing.

Final word
After the surgery, the person goes through psychological stress. Your physiotherapist has many roles, not only to come out of physical disability but also to motivate you in every step of rehabilitation. Rehabilitation should emphasize the return to functional abilities.
The author is a physiotherapist who has been practising for the last 17 years. He owns a successful physiotherapy clinic named "Physiofirst" in Rourkela, Odisha, India.
He holds a Bachelor's in Physiotherapy (BPT) from SVNIRTAR (Swami Vivekananda National Institute of Rehabilitation and Research), one of the prestigious physiotherapy schools in India.
Taking every pain and disability case as a challenge is his motto. Whatever he learns dealing with his patient, he shares it with the world through blogs and e-books.
He also owns a blog, www.physiosunit.com and a YouTube channel, "Sunit Physiotherapist" with over 8 lakh active subscribers. Here, he shares everything he gets to learn serving the patient. His knowledge and invaluable experience in the field are proving beneficial to many.
Email him: sunitekka@gmail.com
Phone: +91-9178817004
Join him: www.facebook.com/physiocapsule

Very useful but why money for download.
Hello friend. The problem is you mention in this article is well worth a look. Very helpful article. Like
John