Last updated on February 27th, 2025 at 04:51 pm

Let me start with one of the case studies I treated in my physiotherapy centre.
An 18-year-old hockey player came for post-operative physiotherapy of a patella fracture. While playing a tournament, he sustained a direct blow over the right patella with the hockey stick of the opponent player.
He was immediately rushed to the local hospital, where, after initial treatment,
Surgery was indicated, and open reduction internal fixation with K-wire fixation was performed. After the operation, the knee was immobilized with a cylindrical plaster cast for one to five weeks.
After removing the plaster cast, he was referred to physiotherapy for further management.
Table of Contents
- Patella fracture rehabilitation exercises simplified
- Physical therapy exercise for broken patella with plaster on
- 1) Active movements of the ankle, foot, toe
- 2) Assisted straight leg raise exercise for broken knee cap
- 3) Knee press exercise (static quadriceps exercise)
- Exercises 3 – 4 weeks after the removal of plaster cast
- 1) Knee flexion-extension on CPM exerciser (Continuous Passive Motion exerciser)
- 2) Active knee flexion-extension physical therapy after patella surgery
- 3) Knee press using pillow or bedroll
- 4) Straight leg raise exercises for fractured patella
- 5) Partial weight-bearing gait using a crutch or cane
- 6) Full weight bearing
- What are the causes of knee cap fracture?
- Patella fracture FAQ
Patella fracture rehabilitation exercises simplified
Though I started this article with a case of a young hockey player, the study papers have a different story.
- The study reveals that patella fractures are more common in females who are 65 years old or above.
- The primary cause of these fractures is minor trauma, and around 70% of cases occur due to falling from a standing height1.
- Most patella fractures are treated without surgery, and only 24% of cases require surgical intervention2.
The treatment for a knee cap bone fracture depends on the type of fracture that has occurred.
- A simple hairline fracture can be treated with posterior slab immobilization for 2 to 3 weeks.
- Surgical intervention is required if the broken segment is displaced due to quadriceps femoris traction.
- ORIF (Open Reduction Internal Fixation) is necessary for fractures with displacements >3mm and articular incongruity of 2mm or more3.
- Tension band wiring is the most common surgical procedure for this fracture type.
After surgery, the leg is immobilized with a cylindrical plaster cast for 3 to 4 weeks.
In both conditions, physiotherapy must start immediately after the leg is put under the cast. During this period of immobilisation, movement of the remaining joint has to be started as early as possible to prevent complications such as joint stiffness, swelling & oedema, and muscle weakness.
Physical therapy exercise for broken patella with plaster on
Whatever exercises I will demonstrate under this subheading are performed when the knee joint is still under the plaster cast. Though the model in the image does not have a knee plastered, we must follow the exercises’ gist.
So, let us start with ankle, foot, and toe movements.
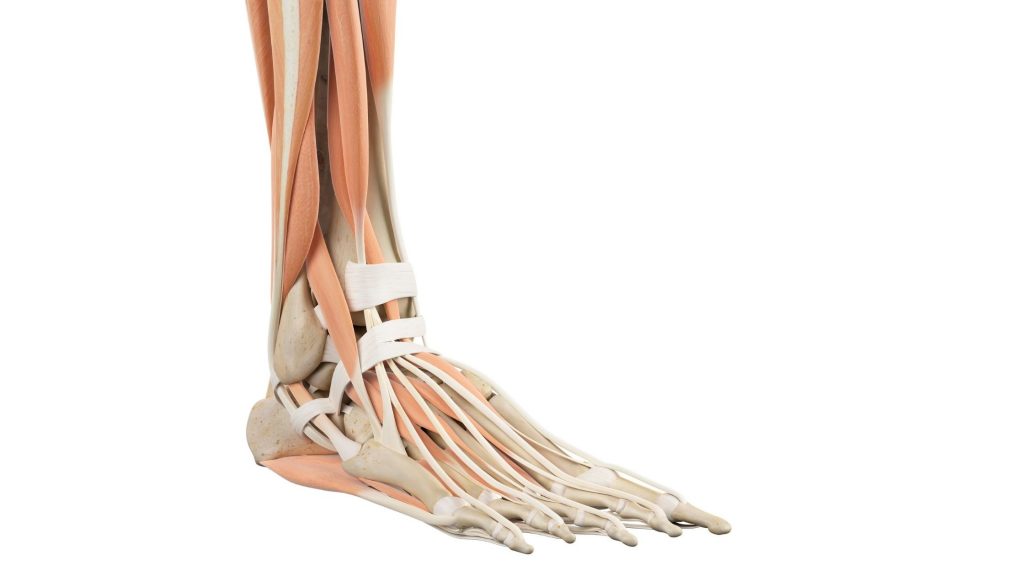
1) Active movements of the ankle, foot, toe
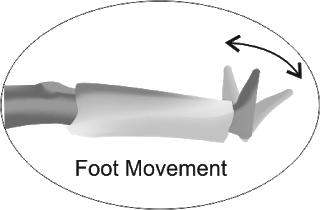
This exercise is very important to maintain the blood circulation around the lower leg and prevent oedema.
It also helps maintain the flexibility of the muscle and other soft tissues around the lower leg and foot. Here’s the step-by-step process for performing this exercise.
- Sit comfortably in a long sitting posture.
- Move your ankle, foot, and toe up and down.
- Perform the movement as many times as possible and whenever possible.
- Move both the ankle joint and toes.
2) Assisted straight leg raise exercise for broken knee cap

Our next exercise is an active-assisted straight leg raise. This exercise requires a partner to assist you in raising your leg straight up to 30 degrees of angle.
It’s important to note that this exercise should not be entirely passive but rather an active movement with some assistance. It is an effective way to strengthen the muscles in your legs and improve flexibility. To perform this exercise:
- You will need to lie down on your back with your partner standing next to you.
- Your partner will then hold onto your leg just above your ankle.
- Keep your leg straight and lift it up towards the ceiling, as high as you can go with some outside help.
- It’s important to maintain the active movement of your leg while your partner assists you.
- For maximum benefit, you should aim to repeat this exercise a minimum of 10 to 15 times per session.
3) Knee press exercise (static quadriceps exercise)
This exercise is designed to help strengthen the quadriceps muscle in the front of your thigh, which can be weakened after a knee cap fracture. To perform this exercise:
- Sit on the bed with your legs extended in front of you.
- Keep your back straight and your hands resting on your thighs.
- Slowly squeeze your right knee and press it in a downward direction towards the floor.
- Hold this position for 5 seconds.
- Release the pressure. Repeat this for 15 to 20 repetitions of the exercise in each session.
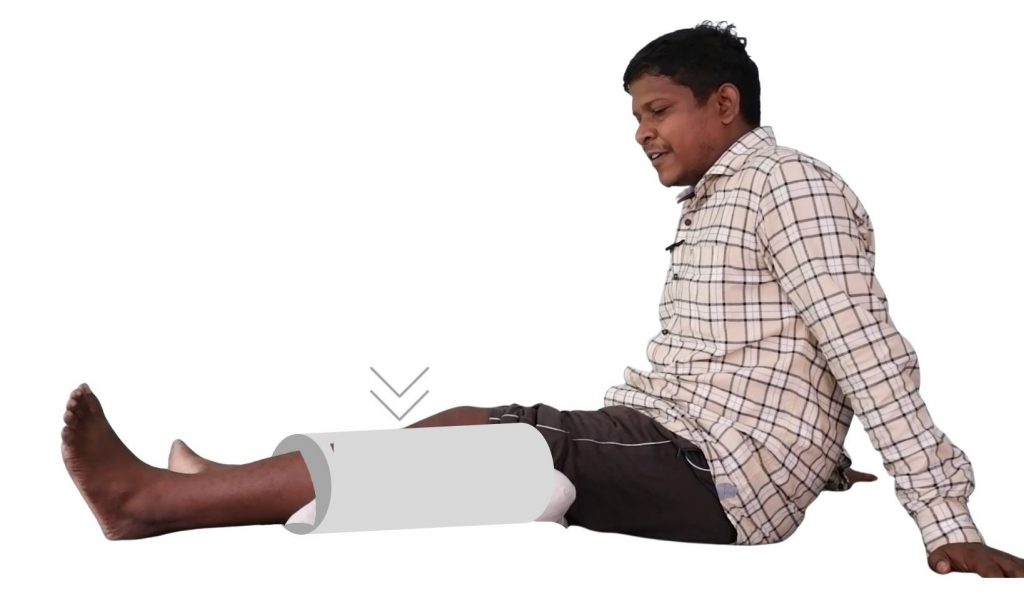
Exercises 3 – 4 weeks after the removal of plaster cast
After 3 -4 weeks of plaster immobilisation of the knee, the sufferer finds that the knee has become stiff. Due to pain and stiffness, it becomes difficult to bend and straighten the knee. There is also a problem with walking.
So, immediately after the plaster removal, careful knee movement had to be started. So, here are the best exercises for fractured patella after removing plaster.
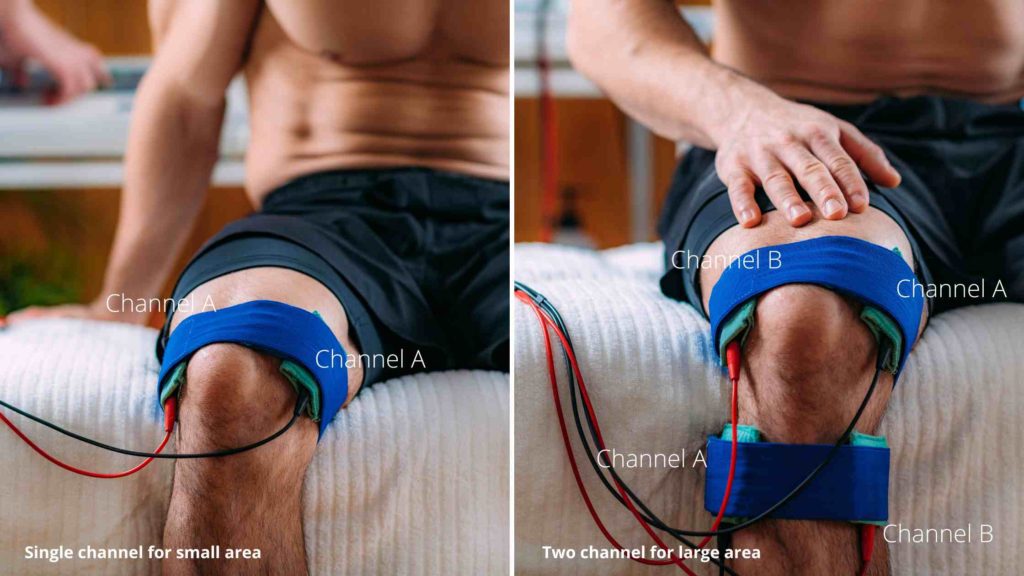
1) Knee flexion-extension on CPM exerciser (Continuous Passive Motion exerciser)

The Continuous Passive Motion (CPM) machine is used to regain knee movement when there is still a lot of pain around it.
It is a device that fixes the knee in place, as shown in the figure, and has a graduated angle control that can be used to increase the angle of movement.
Once the knee is properly fixed, the machine is set to bend it passively within the pain-tolerable range. If knee bending is painful, the machine reduces the bending angle. This way, the angle is slowly increased day by day.
This device can be found at any well-equipped physical therapy centre, and it is always used under the supervision of a qualified physiotherapist.
2) Active knee flexion-extension physical therapy after patella surgery

For this exercise:
- Lie flat on your back with your legs straight out in front of you.
- Slowly bend your knee, bringing your heel towards your buttocks, until you feel a comfortable stretch in the back of your leg.
- Hold this position for 5-10 seconds and then slowly straighten your leg back to the starting position.
- Repeat this movement 10-15 times, ensuring that you are within your pain-free range of motion.
- Gradually increase the range of motion daily, but do not push yourself too hard or fast.
3) Knee press using pillow or bedroll

The knee press exercise is a simple and effective way to strengthen the quadriceps muscle in the front of the thigh. Here are the detailed steps to perform this exercise:
- Sit in a comfortable and long sitting position with your legs straight out in front of you.
- Place a pillow or a bedsheet roll under the affected knee to elevate it slightly.
- Now, contract the quadriceps muscle in the front of your thigh and press down on the pillow with your knee.
- Hold this position for 5 seconds, making sure to keep the rest of your body relaxed.
- Release the pressure on the pillow and relax your leg for 5 seconds.
- Repeat the knee press procedure 30 to 50 times in a single session, depending on your comfort level. Take a break between sets if you feel fatigued, but aim to do as many sets as possible to increase the exercise’s effectiveness.
4) Straight leg raise exercises for fractured patella

The exercise described is a strengthening exercise for the quadriceps muscle and is called the straight leg raise. The following are the steps to perform this exercise:
- Lie down on your back on a flat surface such as a yoga mat or carpet.
- Bend one leg at the knee while keeping the other leg straight.
- Push the back of your knee onto the mat to tighten the muscles in the straight leg. Slowly raise the straight leg to a height of no more than 30 degrees.
- Hold the leg in the raised position for 5 seconds while pushing the back of your knee down onto the mat.
- Slowly lower the leg back down to the starting position.
- Repeat the exercise for a minimum of 10 repetitions on each leg.
5) Partial weight-bearing gait using a crutch or cane
In the first stage, the patient may need crutches or a wheelchair to move around. As the healing process progresses, the patient can begin to bear partial weight on the affected leg while walking with the help of a cane.
This is an essential step towards regaining strength and mobility in the affected leg and can help accelerate the overall recovery.
However, it is essential to follow the guidance of a healthcare professional during the rehabilitation process to ensure a safe and effective recovery.
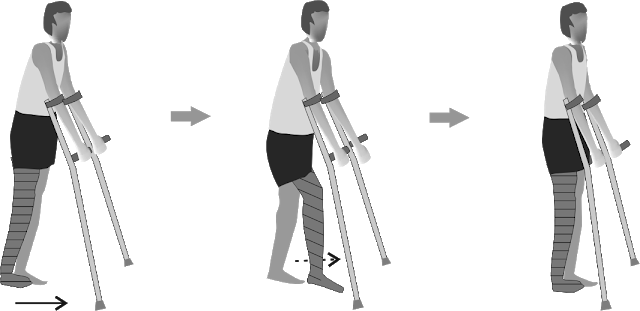
6) Full weight bearing
After a tibia bone fracture, a crucial part of the rehabilitation process is to start independent walking with full weight bearing on the affected leg.
This typically begins around six weeks after the injury, once the bone has had time to heal and the patient has progressed through other rehabilitation exercises.
This step is essential for regaining strength, mobility, and range of motion in the affected leg.
What are the causes of knee cap fracture?
The knee cap or patella fracture can be due to:
- The direct injury occurs with a direct blow on the patella while the
knee is slightly flexed, like falling on the knee or a direct assault on the knee. The above-discussed case is one example of direct injury. - The indirect injury occurs when the knee is bent forcefully while the quadriceps muscle (in the front of the thigh) contracts strongly.
Classification patella fracture
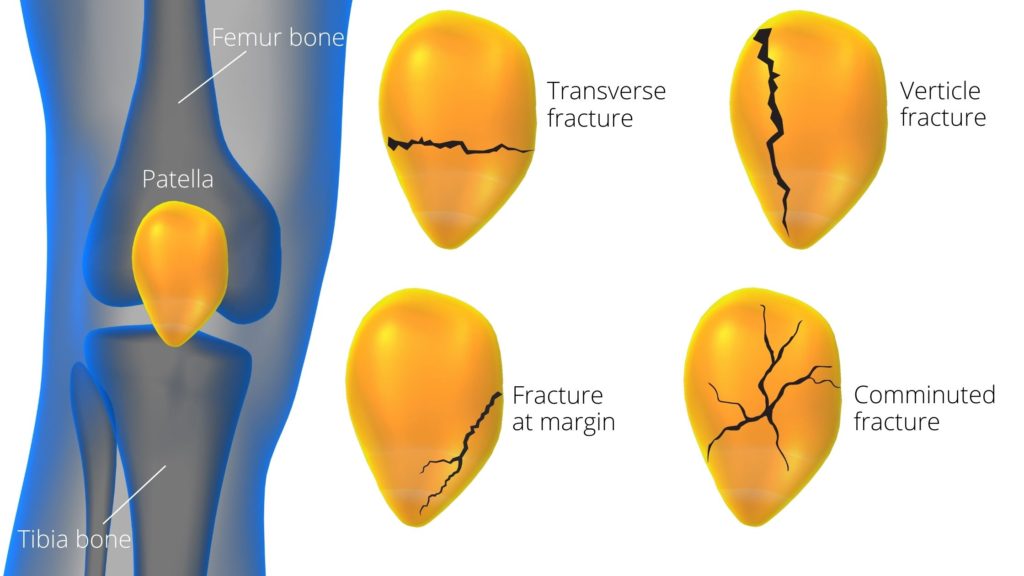
The patella, also known as the knee cap, is a flat bone at the front of the knee. It has a triangular shape, and its edges are rounded, with the apex pointing downwards. The upper base of the patella is connected to the quadriceps tendon.
At the same time, the lower apex is attached to the ligamentum patella, which, in turn, is connected to the tibia bone of the leg.
Traumatic fractures of the patella are classified as transverse, vertical, comminuted, marginal, or osteochondral according to the principle of practice.
- Transverse fracture: This type of fracture occur horizontally across the patella and divides it into the upper and lower part. It is most often due to an indirect impact on the patella, like falls.
- Vertical fractures: Vertical fractures run from the inferior to the superior pole and divide into left and right fractured parts. This type of fracture is generally stable and often treated conservatively without surgery.
- Fractures to the margins of the patella: This fracture occurs at the perimeter of the patella. It commonly happens due to a direct force to the side of the patella.
- Comminuted fractures: The patella, when fractured into multiple segments, is termed a comminuted fracture. It is frequently seen in multiple injured patients.
Clinical features of broken kneecap
- Pain and swelling over the knee. In un-displaced fractures, pain and tenderness are localized to the knee. In a displaced fracture, one may feel the gap between the displaced fracture segments. Swelling is due to hemarthrosis.
- There is a loss of active knee extension.
- X-ray examination: X-ray examination indicates the patella fracture.

Further reading: Exercises for arthritis in knee for pain relief
Patella fracture FAQ
The author is a physiotherapist who has been practising for the last 17 years. He holds a Bachelor's in Physiotherapy (BPT) from SVNIRTAR (Swami Vivekananda National Institute of Rehabilitation and Research), one of the prestigious physiotherapy schools in India.
Whatever he learns dealing with his patient, he shares it with the world through blogs and e-books. He also owns a YouTube channel, "Sunit Physiotherapist" with over 8 lakh active subscribers. Here, he shares everything he gets to learn serving the patient.



Pingback: 9 Best Patella Fracture Recovery Exercises after broken kneecap surgery – Rambam Wellness
I year after dislocating and shattering knee is still difficult climbing and walking without knee brass. Walking seem to cause excessive fatigue and almost passing out , blocking serqulation to my brain . Is that comen and how can I stop it. But when I ware a knee brass I have better mobility. Should I look into knee replacement
Thanks Sunit, much appreciated. We went and saw a physio this afternoon and my wife will start working with her soon!
She can start knee bending after one month under the supervision of a physiotherapist in a CPM machine. And yes she can start exercises and physio with k-wire fixed
Nice article – thanks.
I have a question related to my wife’s fractured Patella. She has k-wire in and tension bands. When time comes to start trying to bend the knee – can she start physio with the k-wires still in place?
Thanks 🙂
You can consider these two exercises described in one of my article here:
1: Straight leg raise in side-lying
2: Adductor strengthening exercise
I have recently fractured my left patella (transversal, no dislocation). The fracture has healed quite well, and knee extension is greatly improving. I am somewhat concerned about the strength of my muscles in the upper leg (vastus medialis and -lateralis?). How I can I work on strength for these muscles without running the risk of putting too much force on the fractured patella?
I read your description carefully and the symptoms you described indicate patella hairline fracture. \You must consult your doctor for confirmatory diagnosis and you can use a knee immobilizer for two weeks to allow the union of fracture if any
Hi there …not sure if this is still active?
63 y.o. Female. Active, gardening, cut grass, walk 2-3 miles per day rain or shine. Walk my dog. Etc.
3 weeks to the day , I was getting dry wood from behind my house for my fire Pitt. I get long dry limps and stomp on them and they break very easily. I went to stomp on the last limb and did not realize there was another limb laying at the end of the limp about 4 inches in diameter.
Symphotainsly when I stomped on the limb, the one on the end came up with great force and WACKED me square across the knee cap! It was daylight, but the stars were out!!! The pain was horrible!
That night I had to get crutches. Pad pain! Could not put weight on leg.
Could not lift leg. Stayed on crutches several days. I forced myself to walk, but pain was very bad. Used a walking stick but could not walk without a great dead of pain for 2 weeks. No matter how much I tried to walk normally, I could not.
Now…although better…still pain each step.
IOW…It was painful and I couldn’t do that….Now I can do that, but it’s painful.
Can not squat, can not go up and down stairs without painful. Very point tender on top of PETELLA.
NEGATIVE for Thessley test. Can not stand on that leg alone with bent Knee.
QUESTION….COULD THIS BE A SLIGHT CRACK IN PETELLA?
Or…..cartilage damage under knee cap?
Thank you…Cindy
Superb sir very nicely explained all exercises
I m also a physiotherapist