Last updated on February 27th, 2025 at 10:17 am

Which is worse, rheumatoid arthritis or osteoarthritis?
Both rheumatoid arthritis and osteoarthritis cause joint pain but are still different. Arthritis, a common term in osteoarthritis and rheumatoid arthritis, is a broad term to describe joint pain. There are more types of arthritis than we commonly know.
There are over 100 types of arthritis, such as osteoarthritis, rheumatoid arthritis, gout, ankylosing spondylitis, systemic lupus erythematosus, osteochondritis dissecans.
Among all arthritis, rheumatoid arthritis and osteoarthritis are the most common. This article will try to understand the difference between rheumatoid arthritis and osteoarthritis.
We will also discuss the signs and symptoms that differentiate them. If you read the article till the end, you can easily find which arthritis is worse.
Rheumatoid arthritis and osteoarthritis
Arthritis is a term that refers to any painful inflammatory joint condition. The term “arthritis” is a combination of two terms, “arthro”, which means joint and “itis”, which means inflammation. This condition can affect any small or large joint, movable or immovable.
The knee and hips are large joints that can be affected by arthritis, while the joints of fingers, toes, and even intervertebral facet joints are examples of minor joints.
Arthritis can also affect immovable joints such as sacroiliac joints around the lower back and rib cage joints. Rheumatoid arthritis (RA) and osteoarthritis (OA) are two common types of arthritis that affect millions of people worldwide.
While both conditions share some similarities, their causes, symptoms, and treatment differ.
Before we discuss the actual difference between rheumatoid arthritis and osteoarthritis, let us first understand the standard definition of the term arthritis.
1) RA vs OA
Osteoarthritis (OA) is a degenerative disease
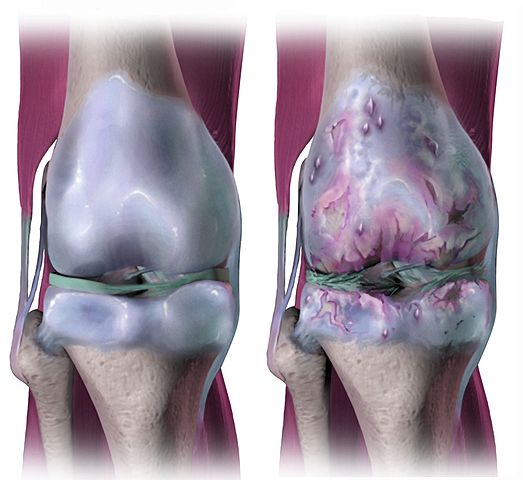
Osteoarthritis is a condition that can damage your joints over time. If you have osteoarthritis in your knee joints, the damage in your knees can increase as you age. We call it a progressive disease.
This condition is unrelated to any internal systemic disease but is more commonly caused by external physical factors. Knee osteoarthritis is a condition that is often caused by repetitive pressure or stress on the knee joint.
For example, individuals who frequently engage in activities requiring getting up from a seated position, standing up repeatedly, or sitting in a squatting or crossed-leg position may be at a higher risk of developing knee osteoarthritis.
This is due to the constant strain on their knees over time.
There are many other reasons why people can develop arthritis in their knees – it’s often found more commonly in old age, and people who are overweight are also at a higher risk. While it is commonly associated with the knees, it can also impact other joints, including the hips and small joints like the thumb.
In fact, finger arthritis is often caused by professions that involve continuously applying pressure through the thumb, such as carpentry, sewing, and typing1.
Rheumatoid arthritis (RA) is an autoimmune disease

Rheumatoid arthritis is a disease that affects multiple joints in the body simultaneously.
Unlike osteoarthritis, which only affects joints under physical pressure, rheumatoid arthritis is a systemic disease that affects small joints throughout the body, including those in the fingers, toes, and larger joints.
This autoimmune disease occurs when the immune system, meant to protect the body, attacks the joints, causing symmetrical joint pain.
For example, if the fingers on the left hand are affected, the fingers on the right hand will also be affected. Similarly, if rheumatoid arthritis affects the right knee, it will also affect the left knee.
In contrast, it is possible to have arthritis in one knee with osteoarthritis and not the other. Rheumatoid arthritis is a chronic inflammatory disease that causes inflammation in all the affected joints.
Also Read: Newly Discovered Gut Bacteria May be Culprit Behind Rheumatoid Arthritis
2) RA vs OA based on its causes
Causes of OA
We cannot point out a single cause of osteoarthritis. Some factors cause it, and a group of people are more likely to develop it. But, again, no single factor is responsible for it. Let us try to understand the factors.
- Old age: Although we usually associate old age with OA, one should not consider this a normal ageing process. There are other factors that, in combination with old age, can be destructive. I have seen (you may also have experienced) that many senior citizens around our society do not suffer from osteoarthritis.
- Overstress on the joints: At the micro-level, repetitive overstress can lead to OA and can be due to a profession that requires work or altered body posture or altered body posture due to an old injury or fracture. For example, a profession requiring repetitive knee bending can lead to OA.
- Obesity: Obesity is a risk factor, but again, we can not single out this factor. This is because there are thin people with OA and obese people who are not suffering from it.
Cause of RA
Its exact cause is unknown and is still a topic of research. But, we can associate a few causative factors with RA.
- Rheumatoid factors (RF): More than 70% of all RA sufferer have been found with RF in their blood.
- Human Leukocyte Antigens (HLA): HLA is found in most human cells and can generate an immune response. In rheumatoid arthritis, it has been found that HLA-D antigens increase.
3) Osteoarthritis vs Rheumatoid arthritis based on their clinical feature, symptoms
Here, we have a comparative study between both types of arthritis, OA and RA, based on different symptoms.
| SYMPTOMS | OA | RA |
| Morning pain & Stiffness | Yes | Yes |
| Involvement of small joint | No | Yes |
| Multiple | No | Yes |
| Symmetrical joint involvement | No | Yes |
| Joint fusion | No | Yes |
Clinical features of osteoarthritis
- Joint pain
- Joint stiffness
- Crepitus: Crepitus is the production of a crackling sound when joint moves. An OA sufferer can observe a cracking sound that is produced from the knee when trying to come to stand from sitting or vice versa.
- Bony enlargement is seen around the joints
- Bone becomes tender out of pain.
Clinical features of rheumatoid arthritis
- Usually, the pain starts in the lower back and then extends to small joints of fingers and toes.
- Joint affection is symmetrical. It simply means that if the disease affects the joints of the right thumb (for example), it also affects the opposite side of the thumb joint.
- Morning joint pain and stiffness.
- Joint stiffness develops with the progression of the disease. It affects more small joints, and with time, it also affects spinal joints.
- Nodules formation on joints.
- In very late cases, it affects the large joints like the knee and hips.
- In very late cases, the disease process also affects the joints of the rib cage, leading to respiratory complications, like breathing problems and respiratory infections.
4) RA vs OA based on treatment
The goal of treatment for both RA and OA is to reduce pain, manage symptoms and halt further joint damage. Non-steroidal anti-inflammatory drugs (NSAIDs) are prescribed to help with pain and reduce swelling.
How is osteoarthritis managed?
Conservative management is the first choice of treatment for osteoarthritis joint pain, which includes exercises and mutual protection techniques.
Exercises depend on the affected joint; if you have a knee OA, then you should follow knee osteoarthritis exercises and for hip OA, follow exercises for hip osteoarthritis.
A knee cap or knee brace is also advised in late osteoarthritis cases. I have discussed in length and breadth all the aspects of osteoarthritis knee management in one of my books titled “Combating knee pain naturally.” You can refer to it for in-depth information.
Medication includes analgesics. If the destruction of the joint surface becomes irreversible, the TKR (Total Knee Replacement) is the only option left.
Physical therapy helps to stabilize and strengthen joints. Heat, rest, weight reduction, and massage also help with pain management.
What are the available treatment options for rheumatoid arthritis
People with RA need stronger oral steroid medications, such as prednisone, to manage inflammation. They also use medications that prevent joint destruction and halt disease progression, including biologics and disease-modifying anti-rheumatic drugs or DMARDs (Methotrexate).
A recent study discusses the potential use of hydrogel to manage knee arthritis. This can be a promising treatment for OA shortly.
Regular physiotherapy to prevent joint stiffness and fusion together with Biologics and DMARDs are known for their effectiveness and their increased risk for side effects and infections.
Which is worse, rheumatoid arthritis or osteoarthritis?
Rheumatoid arthritis is much worse than osteoarthritis. RA affects multiple joints. If it affects the joints of the rib cage, it even causes difficulty in breathing. Moreover, I have seen a significant difference in OA people’s lives after replacement surgeries, which is not possible in RA.
Keep Reading: New arthritis drug can stop bone degeneration|Study
Frequently Asked Questions (FAQ) About Rheumatoid Arthritis and Osteoarthritis
The author is a physiotherapist who has been practising for the last 17 years. He holds a Bachelor's in Physiotherapy (BPT) from SVNIRTAR (Swami Vivekananda National Institute of Rehabilitation and Research), one of the prestigious physiotherapy schools in India.
Whatever he learns dealing with his patient, he shares it with the world through blogs and e-books. He also owns a YouTube channel, "Sunit Physiotherapist" with over 8 lakh active subscribers. Here, he shares everything he gets to learn serving the patient.





Pingback: 9 Pictures of the Gout: Symptoms, Food to avoid, other tips - Physiosunit
Hello there Every Buddy! Have you elder folks gone to check out PanGlobalMedicalSupplies.com?
They carry Bathroom Safety Equipment for Seniors,
Fall Prevention for the Elderly, Specialty Wheelchairs and Accessories for people with disabilities and a
lot more. A 1-stop online shop for seniors. Check it out.
You’ll be glad you did.